hematuria and AKI Post transplant
medcases00
Published on Aug 22, 2021
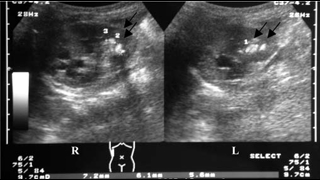
45-year-old male with history of kidney transplant 3 years ago, presents with fever, dysuria, hematuria and acute kidney injury. ( creat was 3.5, was 1.4 2 weeks ago) No recent nausea, emesis, no signs of volume depletion and does not respond to a fluid challenge –on exam he does not have any renal flank tenderness, renal ultrasound shows no evidence of hydronephrosis. Prograf levels normal range and is compliant with IS regimen - 2 years ago was treated for lymphoma with cyclophosphamide. His renal biopsy shows significant interstitial inflammation, urine shows evidence of viral inclusions, but a IHC stain for SV40 was negative –
Likely reason for hematuria and AKI is
1) Adenovirus nephropathy - perform IH stain for adenovirus and check PCR for adenovirus
2) Cyclophosphamide induced hematuria
3) BK virus nephropathy
4) UTI related
Answer is choice 1) adenovirus nephropathy
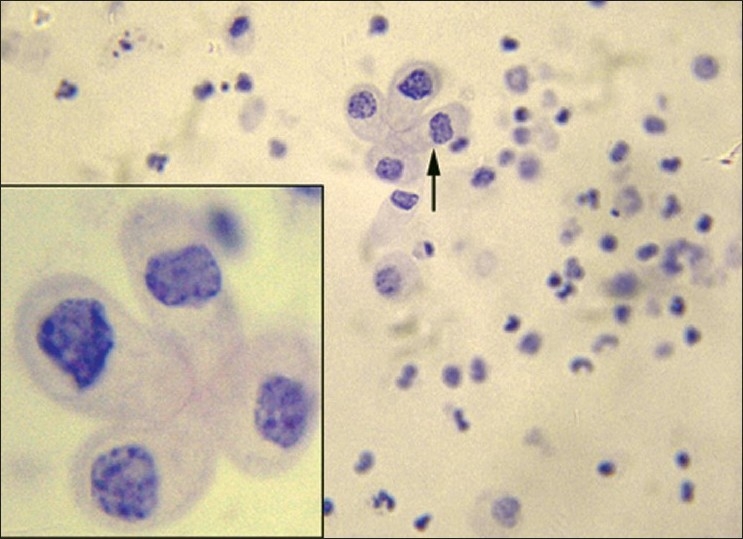
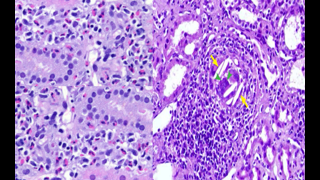
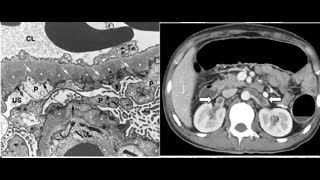
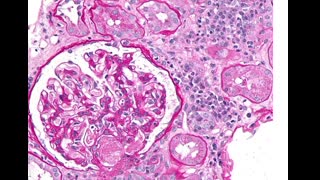
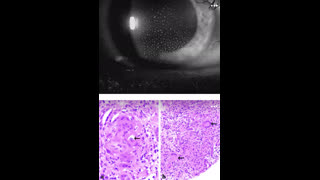
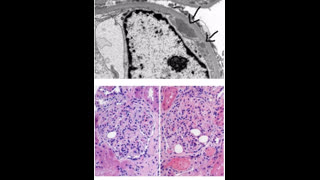
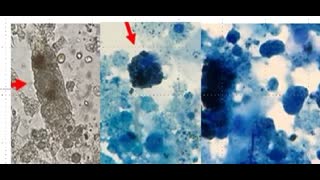
Adenovirus is a double-stranded DNA virus with more than 50 distinct serotypes. Though adenovirus infection is relatively common, adenoviral infection of the renal allograft is rare and also difficult to diagnose if viral inclusions are not present in the biopsy, Urine (see image above, black arrows) also can show nuclear viral inclusion bodies. Based on a limited number of reported cases, patients typically present with fever, hematuria, dysuria, and acute kidney injury. Adenoviremia and viruria are present, as well as decoy cells similar to those seen with BK virus infection. Histology remains the gold standard for the diagnosis of invasive adenovirus infection. Infected tissue typically shows cytopathic inclusions. Necrotizing interstitial nephritis with granuloma formation and prominent macrophage recruitment are also characteristic of renal adenovirus infection. The virus can be confirmed by histochemical staining, or electron microscopy can identify crystalline arrays of adenovirus particles in tubule cell nuclei and cytoplasm. The histologic appearance and histochemical staining can provide a definitive diagnosis of adenovirus, even when cultures and PCR are negative-Management for patient by reduction of immunosuppression followed by intravenous immunoglobulin and cidofovir weekly for 3 weeks. for prominent granulomatous interstitial nephritis on the biopsy, consideration to be given a steroid taper as well. An important side effect of cidofovir is nephrotoxicity, which also can manifest as acute tubular necrosis. Cidofovir therapy in reduces the viral load but may may cause subsequent increase in serum creatinine.
2) cyclophosphamide bladder hemorrhagic cystitis from acrolein toxicity manifests earlier post exposure
3) SV 40 stain was negative making BK virus less likely
4) UTI does not usually cause AKI, unless there is pyelonephritis which is absent clinically or on imaging
Reference
Adenovirus Infections in Transplant Recipients | Clinical Infectious Diseases | Oxford Academic (oup.com)
Adenovirus in solid organ transplant recipients: Guidelines from the American Society of Transplantation Infectious Diseases Community of Practice – PubMed (nih.gov)
Adenovirus in Solid Organ Transplantation – Florescu – 2013 – American Journal of Transplantation – Wiley Online Library